Vaccines were key to curbing COVID-19 in Europe; other measures also useful
Experience in Europe shows that mandatory and voluntary social distancing and economic incentives to increase compliance with emergency measures were critical to bringing the COVID-19 viral reproduction number below 1—indicating one infected person passed the virus to fewer than one other person. However, no single factor can account for the realized outcomes.
Among factors considered, we find that vaccine uptake was the most important in reducing effective transmission rates in 2021, though the other factors helped bring infections under control.
The COVID-19 pandemic has claimed millions of lives, brought about costly government interventions to contain it, and caused unprecedented and widespread economic disruption worldwide. The pandemic has now evolved into an endemic infectious disease amid heated debates on the pros and cons of social distancing and other containment policies, notably in China.
In our recent working paper, upon which this article is based, we examine the evolution of virus transmission rates in selected European countries since the start of the pandemic in early 2020. Although the European countries on which we focus had similar patterns of transmission at the beginning of the pandemic, they ended up with quite different outcomes.
We exploit these differences to learn about the key drivers of the effective reproduction numbers. In particular, we consider factors such as voluntary and government-mandated social distancing, economic support to comply with containment policies, vaccination uptake and virus mutations.
Reproduction numbers, herd immunity and the virus transmission rate
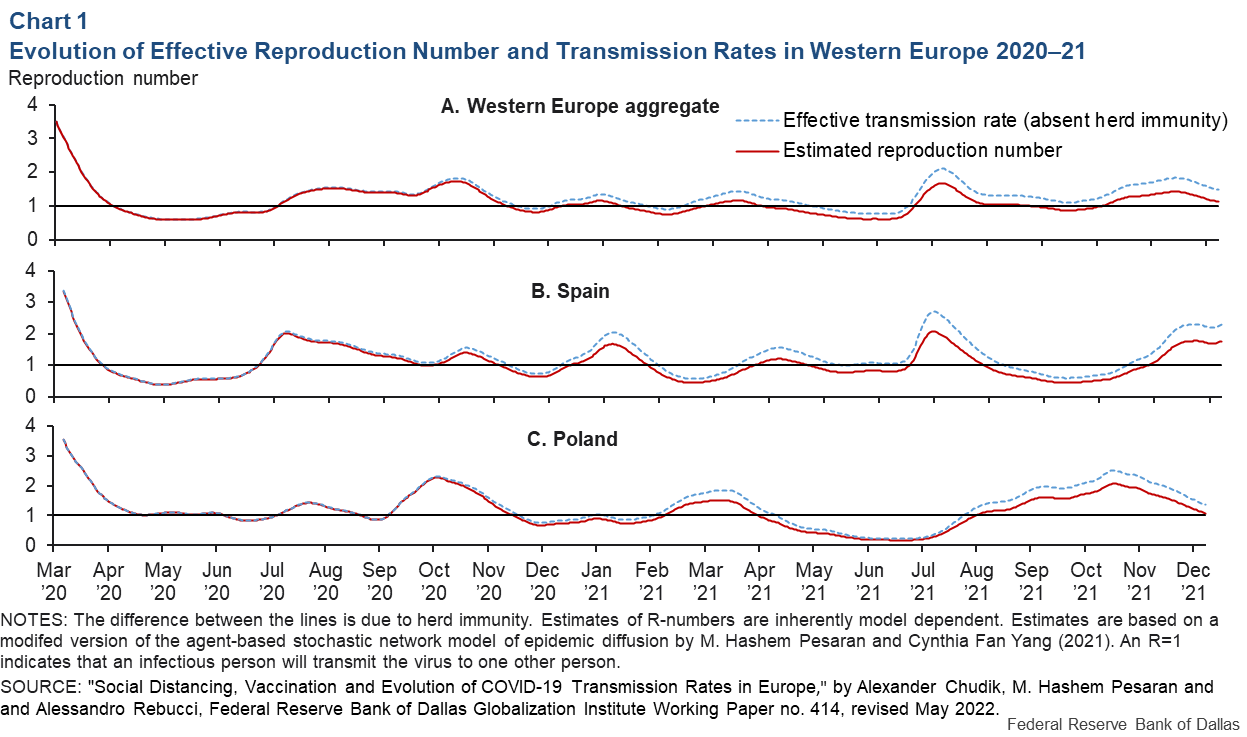
A common epidemiological metric to measure the spread of an infectious disease is the effective reproduction number, the R-number. It measures the new infections expected to result from one infected individual.
Over the past couple of years, this metric has been used widely in the popular press when reporting on the pandemic. An R-number above 1 implies the epidemic is expanding (since one new infection results in more than one expected secondary infection), whereas a value below 1 implies that the epidemic is contracting.
The R-number changes over time (and across countries) due to the shrinking share of susceptible individuals because of immunity following recovery (the so-called herd immunity component) or from a change in the underlying effective transmission rate, which in turn can depend on a multitude of factors mitigating viral spread.
Chart 1A shows our estimates of the R-number for Western Europe as an aggregate (red line) together with a model-implied estimate of what the R-number would have been without any contribution from the herd immunity (dotted blue line), which we broadly refer to as the effective transmission rate. This chart documents a lot of variation—six distinct waves (marked by the R-number exceeding 1)—during 2020–21.
These estimates, however, mask often large differences in outcomes (number of new cases, hospitalizations and deaths) across countries, as shown in panels 1B (Spain) and 1C (Poland).
Determinants of effective transmission rate
Using a panel data approach, we exploit both time-series and cross-country variations in the rate of transmissions to identify the relative importance of different factors affecting the evolution the epidemic in Western Europe.
Changes to the transmission rate are governed by many factors, both biological and behavioral, such as mutations; social distancing (voluntary or mandatory); government-mandated mobility restrictions and compliance with mandated measures; and immunity changes due to vaccination.
We focus on five key factors. To proxy mandated social distancing and incentives, we use the aggregate stringency and economic support indexes compiled by the Oxford COVID-19 Government Response Tracker project for the first two factors.
To assess the potential impact of voluntary social distancing, we allow for “threshold effects” (the third factor), which captures how the fear of becoming infected, stoked by news of increasing cases, influenced individual precautionary behavior. Vaccine availability and public vaccination uptake became more prominent in 2021. We proxy that development by adding the population share of vaccinated people to our panel regressions as a fourth factor.
Our sample ends in November 2021, before the onset of the dominant omicron variant. To proxy for important virus mutations during our sample period, we add the then-dominant delta variant share of the confirmed sequenced cases as our fifth factor.
Statistical significance of transmission rate determinants
We find that all determinants of the transmission rate as proxied by our variables are statistically highly significant and have the expected signs (Chart 2). Before the onset of vaccination, mandated containment policies, incentives to comply with them and voluntary changes in behavior arising from fear of infection were important in bringing down the R-number below 1 over sustained periods.
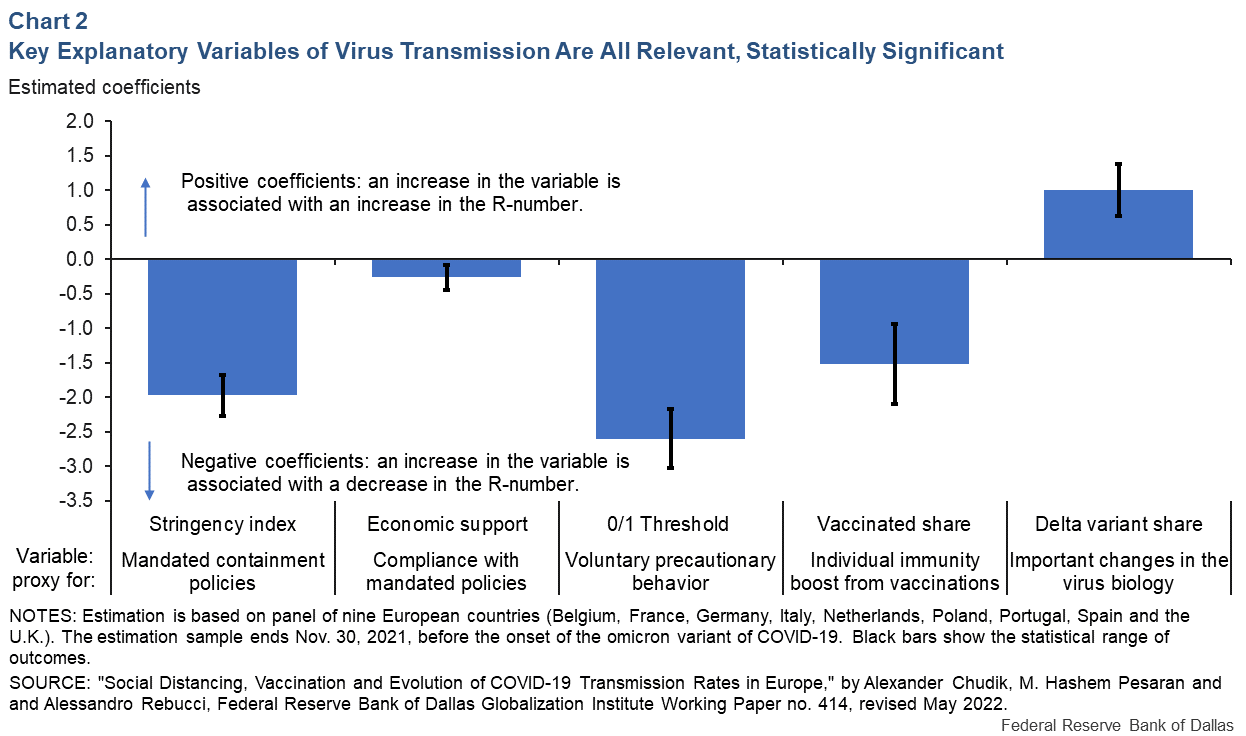
Following the widespread use of vaccination and toward the end of our sample period in November 2021, we find that the degree of vaccine uptake is the most important contributor to the decline in the effective transmission rate.
The delta variant in the spring/summer of 2021 contributed to an increase in the R-number by about 1, which is substantial. Our country-specific estimates of the basic reproduction number (defined as the R-number in a fully susceptible population in the absence of any mitigation measures) are surprisingly similar across countries, in a tight range from 5.1 to 5.5, with a pooled estimate of 5.3. These estimates are much larger compared with earlier estimates found in the literature that range between 3.0 and 4.0.
As with most empirical research, our analysis has its limitations due largely to data issues. An elephant in the room is the accuracy of the reported number of infected cases and the measurement of mitigating factors used in our study. Infected cases are generally underreported, possibly by a factor of 2 to about 7, depending on the period and the country involved.
In our estimations, we allowed for underreporting of the number of infected cases and found that the results are robust to different assumptions on the magnitude of underreporting and its changes over time as availability of testing increased.
Our proxy variables are also imperfect measures. In addition, the availability of data and the related choice of using aggregate (country-level) data necessitate keeping regression specifications parsimonious, which means that we cannot separately examine each of the specific containment policies adopted.
About the Authors
The views expressed are those of the authors and should not be attributed to the Federal Reserve Bank of Dallas or the Federal Reserve System.